A research team led by Elaine Leung Lai Han, professor in the Faculty of Health Sciences (FHS) at the University of Macau (UM), has unveiled critical insights into the responding phenotype of the effectiveness of immune checkpoint blockade (ICB) therapy for non-small cell lung cancer (NSCLC) patients. They identified a set of immune subtypes that are enriched in non-responders to ICB therapy, which can provide a non-invasive and feasible method for early and timely monitoring of treatment response. The research results have been published in the renowned journal Nature Communications.
Although ICB therapy is known to produce durable clinical responses in a selected group of NSCLC patients, not all patients can benefit from it. Therefore, early identification of progression is crucial for treatment selection for patients. To achieve better effectiveness with ICB therapy, parameters indicating favourable response are critically needed. Several predictors of the response to programmed death-1 (PD-1) blockade have been reported, such as the presence of tumour-infiltrating T cells, high programmed death-ligand 1 (PD-L1) expression in biopsies, microsatellite instability (MSI), Kelch-like ECH-associated protein 1 (KEAP1) and Serine/Threonine kinase 11 (STK11) mutations test and the tumour mutational burden (TMB). However, these parameters are hampered by the limited longitudinal observation window, the small number of parameters, and the lack of systematic, unbiased bioinformatic pipelines, which has resulted in a paucity of indicators predicting response state to date. Longitudinal investigation is important to trace markers associated with acquired resistance since the anti-PD1-mediated immune response is dynamic during treatment cycles. Currently, it is unclear whether non-invasive approaches, such as peripheral blood mononuclear cell (PBMC) profiling, can be used to predict responses to ICB therapy by identifying the relevant responding cell types. Prof Leung’s research team has made a breakthrough and their study provides new insights for understanding the underlying immunological mechanisms of primary and acquired resistance.
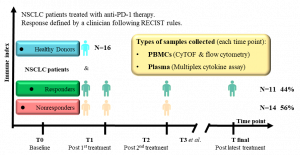
The study followed 25 NSCLC patients for at least 30 months and used innovative high-dimensional CyTOF and multiplex cytokine approaches to examine patients’ blood samples. This allowed the researchers to gain insights into immune populations, their molecular profiles, and functional characteristics. By analysing immune cell responses, the research team identified key markers that can predict the efficacy of anti-PD-1 therapy. The study discovered that the presence of specific immune cell subsets, in particular CD8+CD101hiTIM3+ (CCT T) cells, can predict treatment efficacy. The findings have far-reaching implications for the future development of NSCLC treatment. By utilising advanced techniques to analyse the immune response, the researchers have identified novel predictive markers for treatment efficacy. These insights shed light on precision therapy and contribute to a better understanding of treatment resistance mechanisms.
Prof Leung, Prof Liu Liang at the Second Affiliated Hospital of the Guangzhou University of Chinese Medicine, and Cao Yabing, a doctor at Kiang Wu Hospital in Macao, are the co-corresponding authors. Prof Leung, Prof Li Run-Ze at the Second Affiliated Hospital of the Guangzhou University of Chinese Medicine, and Prof Fan Xing-Xing at the Macau University of Science and Technology share the first authorship. The research project was supported by the Science and Technology Development Fund of the Macao SAR (File no: 0063/2022/A2 and 001/2020/ALC), 2020 ‘Qi-Huang’ Young Scholar programme of the National Administration of Traditional Chinese Medicine, Janssen Therapeutic Fund (File no: ICD#1101175), 2020 Guangdong Provincial Science and Technology Innovation Strategy Special Fund of the Guangdong-Hong Kong-Macao Joint Lab (File no: 2020B1212030006), Start-up Research Grant of UM (File no: SRG2022-00020-FHS), Faculty of Health Sciences of UM (File no: 82204677), Science and Technology Projects in Guangzhou (File no: SL2022A04J00459), and Technology Research Projects of State Key Laboratory of Dampness Syndrome of Chinese Medicine (File no: SZ2022KF20). The full version of the research paper can be viewed at https://www.nature.com/articles/s41467-023-40631-0.
|
Source: Faculty of Health Sciences |
|
|
Media Contact Information: |
|
|
Communications Office, University of Macau |
|
|
Albee Lei |
Tel: (853) 8822 8004 |
|
Jason Leong |
Tel: (853) 8822 8322 |
|
Email: |
|

Elaine Leung Lai Han
The presence of specific immune cell subsets, in particular CD8+CD101hiTIM3+ (CCT T) cells, can predict treatment efficacy
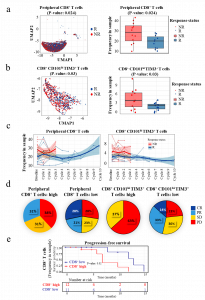
The levels of Granzyme B, T-bet, and KLRG1 are remarkably upregulated in responder CD8+ and CCT T cells, suggesting a possible correlation with positive treatment outcomes
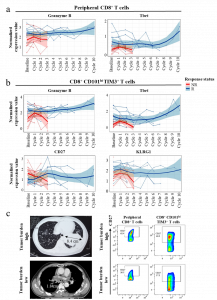
The research team identifies new predictive markers for treatment efficacy by using advanced techniques to analyse immune responses
